Comes, black as a porpus.
The diabolus ipse,
Call'd Cholery Morphus;
Who with horns, hoofs, and tail, croaks for carrion to feed him,
Tho' being a Devil, no one never has seed him!
Ah! then my dear honies,
There's no cure for you. [Samuel Taylor Coleridge, "Cholera Cured Beforehand" (Complete Works, 830)]
King Cholera
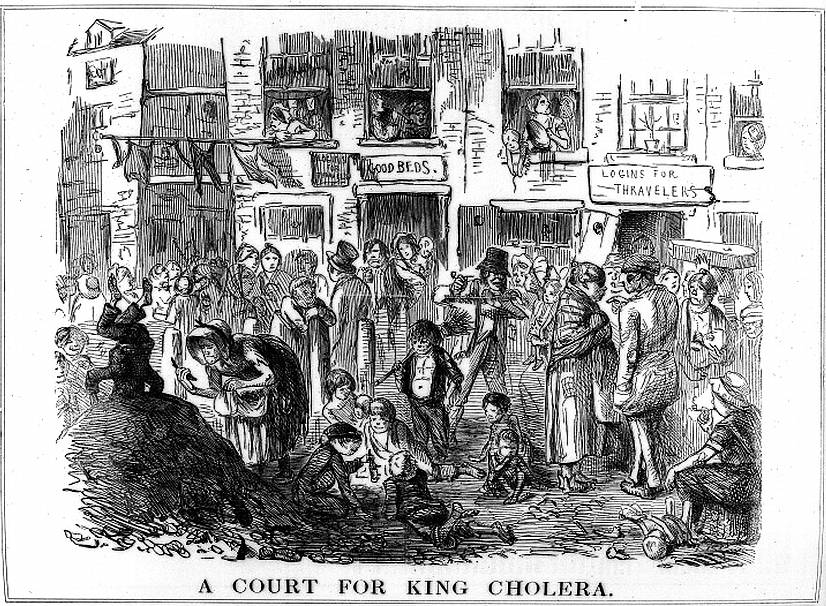
John Leech's cartoon in Punch, 23 (25 September 1852): 139), showing the association of cholera with squalor. A child stands on his head on top of a rubbish heap in the left-hand corner. An old woman scavenges from the heap, another child shows off his own find, and washing flutters in the breeze overhead. Credit: Wellcome Library, London. Many thanks to the Wellcome Library, London, which kindly allows images from its Digital Gallery to be used under this Creative Commons License for educational and non-commercial purposes. [Click on the image to enlarge it.]
Cholera, one of the great scourges of the newly urbanised west in the nineteenth century, is dramatic in its onset, agonising, utterly prostrating and often fatal. Where people live cheek by jowl in unsanitary conditions like those shown in John Leech's cartoon above, it can cut a swathe through a neighbourhood in days. This dreaded disease, whose Greek name means "yellow bile," first came to public notice in 1817. It stalked the world, as Coleridge said it did, like the devil himself. Winding its way inexorably from the vast mangrove swamps of the Sunderbans on the Bay of Bengal, it followed the trade routes and arrived in England in the autumn of 1831, as part of the second great pandemic of 1829-1851. There were to be two further epidemics here, in 1848-49 and 1853-54, the latter during the third pandemic that started in 1852 and continued until 1859 (see Hamlin's Prologue). The one in the late 1840s killed 14,789 people in London alone (White 50).
No one had known how to halt the disease's progress from the east, or how to stop the outbreaks once they started, because no one knew what caused it. Was it contagious? Earlier in 1831 Dr.Calaw, a physician in Berlin, had tested the possibility by performing "some very disgusting experiments upon his own person" (qtd. in Hempel 27). He had promptly contracted it, and died. Yet it did not seem to be passed by ordinary contact. Doctors were able to attend their patients with impunity. When it first arrived in Europe, by far the most commonly held theory was that it was due to contaminated air, or miasma. In England. this theory was held by no less a person than Edwin Chadwick, who in 1832 became assistant commissioner on the Poor Law commission. His Poor Law Commissioners' report of 1842 strongly recommended the removal of human waste, and good ventilation. Suggested preventative measures included heavy ingestion of garlic, burning tar, and dousing the surroundings with chloride of lime. Individuals might also fortify themselves by (for example) wearing flannel girdles and praying. A surprising number put their trust in homeopathy. In light of the fact that the disease spread most rapidly among the lower orders, sobriety and a moderate diet were considered helpful as well.
What was to be done if someone did succumb? Dr Thomas Latta, now hailed as the father of intravenous infusion therapy, had the right idea early on: his "pioneering use of intravenous saline infusion succeeded in rescuing at least some cholera victims from a certain death" (MacGillivray s5). But his voice went largely unheard — partly because he died tragically young in his thirties, of that other devastating but more insidious nineteenth-century scourge, tuberculosis. This was in 1833. In the same year, William Twining (1790-1835), a member of the Royal College of Surgeons, published his own recommendations for treatment. He was serving as first Assistant Surgeon at the General Hospital in Calcutta (see Harrison 173). He wanted to pass on his experiences in treating cholera victims to his fellow-doctors at home, who were facing their first cases. Among the medicines he recommended were camphor and mercury (see 40, 211). More important was bleeding:: "Nothing relieves the spasms of the early stage of febrile Cholera, so effectually as the lancet," he says (65). Another possible measure was to wash out the patient's intestines:
I have also tried Enemas of four and six pints of hot water, containing Ammonia in solution; with the view of stimulating the system and at the same time of washing away from the great intestines the tenacious paste-like secretion which they contain. These Enemas were employed only in the most hopeless cases when other stimuli had failed; therefore they were generally unsuccessful. (70)
Other remedies touted at this time were passing steam over the patient or pouring boiling water on the patient's stomach (see Hempel 46-47). It seems incredible that even a single sufferer should have survived such brutal medical interventions, often involving not the replacement of liquids but the further withdrawing of them, or the application of scalding ones.
Related Material
- Cholera and the Komma Bacillus of Koch
- John Snow and Waterborne Diseases
- Chadwick's Report on Sanitary Conditions
- "The New and Fatal Disease" — Thomas Arnold and the 1832 Cholera
- "Cholera in England and America 1855" (see especially the last two paragraphs)
- A melancholy monument to the ravages of disease in British India
Sources
Coleridge, Samuel Taylor. The Complete Works. Internet Archive. Web. 2 July 2012.
Hamlin, Christopher. Cholera: The Biography. Oxford: Oxford University Press, 2009. Print.
Hempel, Sandra. The Strange Case of the Broad Street Pump: John Snow and the Mystery of Cholera. Berkley and Los Angeles: University of California Press, 2007.Constable, 1988. (Previously published by Granta in 2006, under the title of The Medical Detective: John Snow and the Mystery of Cholera.) Print.
MacGillivray, Neil. Dr. Thomas Latta: The Father of Intravenous Infusion Therapy." Journal of Infection Prevention. 10, Supplement 1 (Sept. 2009).: s3-s5.
Twining, William. A Practical Account of Epidemic Cholera, and of the Treatment Requisite in the Various Modifications of That Disease. London: Parbury Allen & Co., 1833. Internet Archive. Web. 6 July 2012.
White, Jerry. London in the Nineteenth Century: "A Human Awful Wonder of God." London: Cape, 2007. Print.
Last modified 19 January 2017