
y the mid-1850s, zinc chloride paste had become an alternative, or complement, to conventional cancer surgery. Among the prominent physicians who were utilizing ZnCl2 in this period was the American surgeon, Jesse Weldon Fell (1819-1889). Dr. Fell proclaimed that he had invented a novel escharotic method. Despite his efforts to establish the legitimacy of his work in America and later in England, from 1844 to 1857 a controversy overshadowed his practice. Significant questions arose regarding his motives, the veracity of his claims, and the effectiveness of his chemical treatment of breast and skin cancer.
Background, Methods, & Motives
After relocating his family to New York City in 1842, Jesse Y. Fell enrolled in the University Medical College of New York University (UMC/NYU) and graduated with a medical degree in 1844 ("General Alumni Catalogue," 5). While a medical practitioner in New York City, he was one of the founders of the New York Academy of Medicine (NYAM), established in 1847. On 13 January 1847, Dr. Fell became an official member of the NYAM and, at its 24 February meeting, was appointed temporary Librarian. However, on 5 July 1848, he tendered his resignation as an Academy Fellow (Farrow 181). On 2 August 1848, for reasons not immediately clear, his resignation was tabled and forwarded to the Academy’s Committee of Medical Ethics. It had come to light that he had collaborated, in 1847, with a certain Dr. Gilbert in the administration of an unregulated cancer remedy. His membership in the organization, after a contentious seven years, was terminated on 2 January 1856 (Farrow 183; Croft 149-150). After experiencing a number of personal tragedies, Dr. Fell remarried and moved to London where he established a clinic. It is unclear as to whether zinc chloride, some other agent, or a combination, were being administered in the clinic that Drs. Fell and Gilbert had been running.
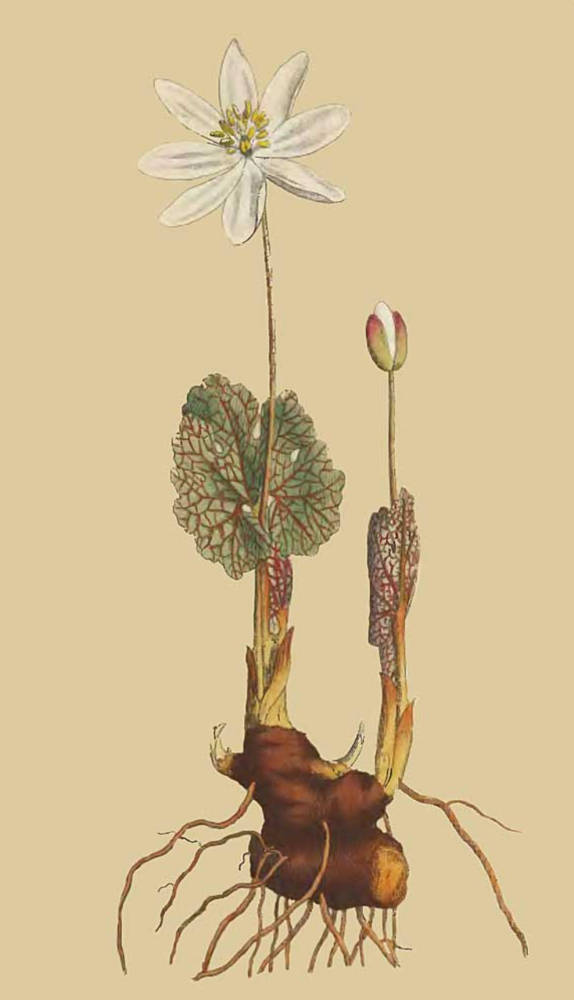
Sanguinaria canadensis or Bloodwort (or Bloodroot). Source: Project Gutenberg version of The Botanical Magazine via Wikipedia. Click on image to enlarge it.
Dr. Fell understood that, for the medical community to authorize its employment, he had to prove its value clinically and to preclude misjudgments based on incorrect applications of the regimen (Farrow 185). In order to satisfy these requirements and to qualify for a patent, he attempted to convince the Governors of Middlesex Hospital, London, that a cancer trial was warranted. After the investigation was completed, he promised to disclose the composition of his remedy and to present evidence of its effectiveness. Fell’s claim for originality rested solely on the use of a Native American remedy, indigenous to tribal cultures of the Lake Superior region. His ointment, combining the alkaloid root-extract of the Sanguinaria canadensis plant (a.k.a. bloodroot [vernacular] or puccoon [Native term]) with presumably inactive ingredients, was to be applied to skin ulcers and malignant tumors (figure 1). In December, 1856, while at Warwick Square, London, he prepared to submit his proposal to Middlesex Hospital.
As noted above, the remedial agent Dr. Fell utilized in his paste, an extract from the S. canadensis plant, was indigenous to North America and had been an element of the Native American pharmacopeia among the Lake Superior, Cheyenne tribes (Fell 56-57). The rhizome’s extract, it turned out, was not very exotic. Its pharmaceutical history, in fact, indicated its properties were very well known: it had been traditionally used as an emetic, expectorant, and, in droplet doses, as a diaphoretic, narcotic, sedative, stimulant, and alterative, as well as an emmenagogue (Gibb 90; Fetrow and Avila 73-4). In 1860, as George D. Gibb, M.D. attests, in a paper read before the Medical Society of London, S. canadensis the extract had no effect on cancer: “As for [bloodroot’s] asserted value in promoting the disappearance of tumors and the cure of cancers, there is not the slightest evidence to favor such a view" (90). Whereas pharmacologists were certain that S. canadensis could destroy fungal growths and was a topical treatment for "obstinate cutaneous affections," Dr. Fell insisted that, over a period of months, it could remove external tumors. Without supporting evidence, however, he made the controversial assertion that it left "the patient cured" (Wood and Bache 648; Gibb 58).
In the early stages of his application to Middlesex Hospital and during the trial, Dr. Fell avoided full disclosure of the ingredients to the Hospital Governors, to the medical community, and to the public. Despite his sensitivity on the issue, he was granted permission to proceed with the tests, and said he would honor his contractual obligation to reveal the escharotic's composition post-trial. It is not clear whether he had confided to his Middlesex colleagues about the full composition of the paste, although it is a possibility. Drs. Campbell Grieg De Morgan (1811-1876) and Charles Hewitt Moore (1821-1870), along with other members of the Surgical Staff, endorsed the experiment (Preface, A Treatise on Cancer, ix-xi).
In the 1857 Treatise, Dr. Fell finally divulged the truth: his escharotic was, in reality, a dual-action preparation, combining the plant alkaloid, which he had maintained was a coagulant, with ZnCl2 or zincane, included surreptitiously to ensure success. Hence, a bloodroot-zincane compound, rather than bloodroot alone, was responsible for removing "large ulcerated tumours" in a few weeks, "with comparatively little, and in many cases [with] no pain"; oral doses of the compound, he proclaimed, could mitigate internal disease (58). But why had Dr. Fell made a false claim about S. canadensis while not identifying the chloride? The motive was likely a pecuniary one: full disclosure during the application period would have dispelled the formula’s novelty and mystique. Fell knew very well that a hospital was unlikely to authorize a trial for a zinc chloride paste since it had been in use since the 1830s. Thus, had Fell revealed that zincane was the catalyst while the trial was active, his mendacity would have been exposed.
Like most surgeons of the period, Dr. Fell knew the history of escharotic medicine, especially as a treatment modality in oncology. An encyclopedic resource, Dr. Jonathan Pereira’s The Elements of materia medica and Therapeutics (1854-1857) traced the chloride’s history, from its ostensible introduction into clinical practice by J. W. Papenguth, to its endorsement by Häncke, and to its development as a treatment modality by Canquoin (772). To indicate the unbroken continuity of the method, Pereira paraphrased Dr. P. F. W. Vogt's (1786-1861) respected assessment. In the 1854 Lehrbuch der Pharmacodynamik, Vogt approved of zincane’s effectiveness, despite the discomfort: "[it] decomposes the organic tissues as quickly as nitrate of silver, but excites more burning, and for a longer time, owing to its action extending to parts placed more deeply . . . . To this circumstance is owing, in great part, the efficacy of the chloride in various diseases in which it has been applied, and the healthy appearance of the sore after the separation of the eschar. There is no danger of any constitutional disorder arising from the absorption of the poison, as is the case with the arsenical and mercurial caustics" (quoted by Pereira, 773-774). At the time of Dr. Fell’s practice, ZnCl2, though transiently painful, was recognized as the most effective and least toxic cancer escharotic on the market. Further proof of its good standing as an escharotic paste can be found in the 1866 Manual of Materia Medica. In this standard source, zinc chloride is recommended as a caustic remedy for a variety of skin disorders: "it is principally employed at the present time to destroy parts affected with intractable forms of disease such as canceroid, old syphilitic, or scrofulous ulcers, and condylomata, the cuticle having been first destroyed by caustic potash. The benefit is supposed not to depend merely on the escharotic effect, but on the chloride inducing a new action in the surrounding parts" (Farre, Bentley, and Warrington, 223).
Dr. Fell had to know that, if the furtive scheme were exposed, then genuine results achieved by the zincane would have been questioned and the escharotic method generally discredited. This is precisely what happened in 1857, as critics accused him of profiteering, false advertising, self-promotion, and quackery. The ensuing scandal had the collateral effect of tarnishing the reputation of physicians who had being employing the product openly. Throughout the late 19th and early 20th centuries, botanicals such as S. canadensis had been excluded from the standard pharmacopeia and their worth derogated. Current biomedical research involving botanical alkaloids, however, has had promising results in oncology. Although S. canadensis cancer salves are controversial and have never been evaluated in clinical trials, the use of the eight S. canadensis alkaloids found in these preparations are being studied more closely (Croaker, et al.).
Dr. Fell’s escharotic procedure was nothing new. The surgeon began by destroying the outer layer of skin with nitric acid and then applying ZnCl2-bloodroot in a matrix of water and wheat-flour, whipped to the consistency of treacle; the skin had to be blistered in this way so that the active ingredient(s) could be absorbed into the tumor (A Treatise, 59). To form eschars, layer-by-layer, was time consuming, so the process extended over months. To increase permeability further, Fell, like John O. Justamond, M. D., incised the affected surface, separating each cut by one-half inch, and being careful not to cut into healthy tissue; spreading paste on cotton strips, he inserted them into the incisions on a daily basis (Justamond 369-83). As noted below, Fell misspoke when he considered the method to be to be entirely original (italics by author: 59). Like Canquoin and others, he varied the proportions of active and inactive ingredients in the paste, to achieve the enucleating effect (60).
The Clinical Trial (22 January-18 March 1857)
When Dr. Fell presented his proposal to London’s Middlesex Hospital, he declared that he could completely extirpate a lesion in several weeks. The ZnCl2 and S. canadensis dual-action formula had stunning effects in the short term; however, it is impossible, from published information, to sort out whether one ingredient was more active than the other, whether the botanical alkaloid was inert, or whether they worked synergistically. Witnesses who attributed the rapid enucleation of tumors entirely to the bloodroot were unaware of the fact that zinc chloride did most, if not all, of the work: "the mass falls out in the course of ten or fourteen days afterwards, leaving a flat healthy sore, which generally heals with great rapidity" (A Treatise, 60). Fell, like Canquoin decades earlier, applied the formula to breast cancer when the extent of the tumor "was well marked"; when it had made "some progress"; or when it was "fully developed" but painless and incipient. The implication was that widespread disease could not be treated with the caustic; apparently, Dr. Fell was cognizant of its limitations. The escharotic method, in his opinion, worked best under the described conditions and was able to destroy palpable, axillary lymph nodes.
It is possible that Dr. Fell considered S. canadensis, not as being entirely inert, but rather as an adjuvant. His work with Dr. Gilbert might have suggested as much. Perhaps the S. canadensis was more than just a mask for the chloride? Fell was certainly interested in combining remedies, as is evident from his salve concoctions. For enlarged nodes and secondary tumors, he designed a "brown ointment." Smeared on cotton, this salve contained older ingredients, namely zinc sulfate, S. canadensis, opium extracts, and conium (alcoholic extract of hemlock), infused in a base of cetacean oil and waxy plant extracts (61). Zinc sulfate, not a cancer escharotic, is a mineral supplement employed in certain regions of the world today to treat parasitic lesions, particularly leishmaniasis (M. Gupta, et al.). In alternation with "the brown ointment," at twelve-hour intervals Dr. Fell administered another ointment (iodide of lead in cetacean oil and glycerin). The complementary salves were believed to disperse "incipient" cancerous tumors. Mindful of how corrosive and unpredictable the combined ingredients could be, he seldom exceeded half-grain doses of powdered bloodroot, along with traces (1/16th to 1/20th grain) of iodide of arsenic and 1 grain of cicuta (hemlock) in pill form. An unanswered question deserved attention: did he prescribe oral zincane to patients and, if so, how much did he use? He disclosed having combined the S. canadensis with taraxacum (extract from dandelion root) in a decoction ("cicuta," OED. I: 414; "taraxacum," II: 3237).
In his 1857 book, Dr. Fell vaunted extraordinary outcomes. Over a 24-month period after treatment, according to his statistics, 80%-90% of patients treated with the knife alone suffered recurrence, whereas only 30% of Fell’s patients treated with bloodroot (both reactants?) allegedly returned for secondary treatment (63). Despite the unproven claims, the Surgical Staff at Middlesex Hospital, open-minded about new cancer therapies, evaluated the formula over a five-month period as objectively as possible, from November 1856 to March 1857. About sixty patients with localized breast and skin cancer were being subjected to the bloodroot-ZnCl2 paste. The medical staff reported that the paste had no effect over “the constitutional nature of cancer,” that is, once it had spread from the initial site ("Report of the Surgical Staff," 34). Nor did the oral dosage of S. canadensis extract, administered concurrently, influence patients’ conditions (35). While assessors of Fell’s method inferred that the plant extract exerted "no curative power," they held to the opinion that the bloodroot tincture was useful for ailments other than cancer (36).
Concentrating on the topical effects of the paste, the observers recorded both positive and negative evidence. The paste, for example, did not appear to irritate healthy tissue adjoining the eschar, and it rarely caused swelling, except where a tumor was large ("Report of the Surgical Staff," 36). Over time, however, they noticed that the escharotic method progressed at different rates and with varying effects from patient to patient (37). Worst of all, for some patients, was the sudden, unexpected increase of tumor size; furthermore, as the primary tumor was being methodically reduced by layers, at times, secondary growths appeared. After a few weeks’ treatment under such conditions, the state of the disease could worsen. While tumor growth occasionally increased as treatment was ongoing, in other cases the escharotic method worked as predicted (37). A very promising outcome, observed by the staff at Middlesex in some instances, was the complete destruction of the primary tumor and the diminution of nearby lymph nodes (36-37). Although evidence from this 60-patient cohort was inconclusive, the Surgical Staff clarified several important aspects of the treatment.
Pain management was a difficult problem. Fell’s regimen had drawn criticism for its purported inability to control discomfort. The Middlesex physicians observed that the worst pain was experienced during the treatment of epithelial cancers, especially on the face, where the paste came into contact with ulcerated surfaces; some patients simply could not bear it; so, for them, the treatment ceased ("Report of the Surgical Staff," 39). The chloride was, no doubt, "acutely painful," but its severity lasted only minutes and could be reduced with cold compresses. Where large lesions had to be destroyed, chloroform was used, and the pre-operative surface was "first frozen by the application of mixed ice and salt" (39). Paradoxically, the least painful part of the operation was experienced as the paste excoriated cancerous tissue (39). The sensation felt in the tumor was described as a dull ache (40). The observers testified that no patient subjected to Fell’s paste suffered the kind of violent and unbearable pain often associated with other versions of escharotic therapy, especially those employing arsenic (41). The severest pain was experienced when an eschar separated from the tumor mass. Opiates were ineffective at this stage. The acute uncontrollable pain was blamed on the peeling away of cauterized layer from exposed nerves (41).
The disclosure issue and ambiguous results notwithstanding, Fell’s five-month trial indicated thatS. canadensis-zincane was a potent, early-stage alternative, or complement to, the knife. Moreover, the dual-action therapy did not exclude the knife. For example, the scoring of each untreated stratum of malignant tissue—the small incisions enhancing absorption into diseased tissue--was surgery, albeit minimal. Combining cutaneous surgery with the caustic paste formed an "efficacious" and "manageable" way of treating the cancer because it allowed the operator a degree of foresight and greater control: "The depth, the extent, the rate of advance and the direction of treatment" could be precisely measured. The result of this combined method also meant that, "no form or position of an external tumour" could frustrate treatment ("Report of the Surgical Staff," 42). The use of the scalpel alone was not as efficient. Since the adhesions and extent of the disease rendered some cases unfit for the knife or paste alone, the "method of gradual incision" was found to be most beneficial (43). Within prescribed limits, the Middlesex doctors agreed that the excision-and-paste method hand a place in external cancer treatment. The staff made a practice of evaluating each patient’s condition, adjusting the therapy accordingly (43). One methodological advantage of the gradual insertion of the caustic by incisions had over traditional surgery was that, if cancer recurred during the weeks’-long procedure or post-operatively in scar tissue, the caustic could be re-applied as necessary, without the patient having to go through secondary or tertiary ablation (44).
During the trial, the physicians at Middlesex considered the extent to which the localized disease was either aggravated or controlled, if it had been extirpated, and if, despite the best efforts, it recurred ("Report of the Surgical Staff," 45). One-third of the patients, they later determined, had been more suited to ablation than to experimental procedures. The disease spread, in two cases, while the escharotic was being laboriously applied. Of the ten in whom the primary tumor had been extirpated, in three, cancer had spread in adjoining skin; and one returned after her procedure had healed, having noticed a recurrence. One was sent home for several weeks, her condition being uncertain, while the remaining half of the trial participants were as yet undergoing treatment. The doctors correctly and to assuage the critics advised that, "time only will allow of a complete comparison between the two modes of treatment."
With respect to length of remission, the consensus of the Surgical Staff was that Fell’s excision-and-paste method "was not superior to that by the knife." The statistics for one-third of trial participants were not encouraging. A return of the disease in four out of the fourteen completed cases, and a failure to extirpate it in three others out of a 21-patient cohort, amounted to a 50% failure rate (4 recurrences and 3 hospital-based failures out of 14 completed cases). These dismal results did not support Fell’s advertised claim of having devised "an entirely original mode of treating the disease . . . in all its various forms" (A Treatise, 45; Preface, v). With two-thirds of the patients still being treated, the observers remained as impartial as they could be. As far as recurrence was concerned, traditional surgery, they realized, was equally, if not more, ineffectual; in this regard, at least the newer mode had not been shown to be "inferior to the knife" (45).
Once it became clear that Fell had employed zinc chloride to augment the botanical, the Middlesex staff sought to identify positive aspects of the investigation. Undeniably, the therapy had had immediate benefits. Morbid growths were routinely reduced to eschars which peeled away, revealing healthy tissue, unaffected by the caustic; moreover, inflammation, abscess, and bacterial infections did not complicate recovery. The Staff concluded, surprisingly, that the paste and the paste-incision methods had relatively the same effect on localized skin cancers; but since no details about type and stage of disease were provided, little else could be said ("Report of the Surgical Staff," 46). In terms of innovation, Fell’s therapy raised four interesting possibilities: (1) it seemed less painful than similar methods; (2) zinc chloride concentrations greater than Canquoin’s No. 4 seemed to intensify the cauterizing activity; (3) the bloodroot could possibly enhance the effect of the zinc chloride; (4) and the incised grid presumably increased absorption (46). The question of overall therapeutic value, ultimately, was contingent on whether all or some of these variations worked to extend remission (47). The Middlesex physicians, though frustrated by their inability to control the disease better, were nevertheless reluctant to abandon the system and Fell’s interpretation of it. Despite the poor statistics, this plan, in their estimation, was "a clear advance upon the past, and may not only be itself improved, but may be the way to more extended blessings upon a class of the community not signally distressed"(47).
As a clinical trial, the Middlesex investigation was historically enlightening, even though the findings were indefinite and contradictory. Nonetheless, its value is assessable if compared to two clinical-trial designs: John Lind's 1747 scurvy experiment and the randomized-controlled design, established by a 1943-44 penicillin trial. Ship's surgeon, Dr. James Lind's (1769-1794) scurvy experiment, on board H.M.S. Salisbury, commenced on 20 May 1747 (Lind, Treatise on the Scurvy, 149-153; A. Bhatt). Selecting twelve scurvy patients at different stages of the disease, Lind gave 12 patients the same basic diet, grouped them into 6 pairs, and, over a six-day period, administered to each pair a different dietary supplement: (1) one pair received a quart of cider per day, per man; (2) one, 25 drops of elixir vitriol, three times per day, per man; (3) one, six spoons of vinegar three times, per man; (4) one, measured dosages of imbibed sea water; (5) one, a lemon and 2 oranges per day, per man; and (6) one, an electuary of tamarind and sugar or honey water, per man. Those receiving the citrus fruit and cider, both (1) and (5), improved dramatically. The electuary, which was standard, served as the control. Even though the patient sample was limited and the timeframe brief, Lind determined that an ingredient in the citrus fruit and cider reversed the deficiency. Independently, in 1928, the biochemists Drs. Charles Glenn King (1896-1988) and Albert Szent-Györgi (1893-1986) discovered ascorbic acid (Vitamin C) (J. Halver and N. Scrimshaw; K. J. Carpenter, resp.).
Lind had owed the success of his experiment, in large part, to the use of six variables, governed by the implied hypothesis that fresh fruit (among other wholesome food) was absent from the naval diet. His simple, but highly effective, experiment was a prototype of the modern randomized-controlled trial. The basic modern design, introduced in 1943-44, has six components (1) at least two or more distinct groups of patients are assembled; (2) assignment to each group is determined by computerized analysis, based on factors such as age, gender, ethnicity, and type, subtype and stage of disease; (3) a control group receives the standard, not the novel, mode of treatment (or a placebo if no standard exists); (4) patients, other than those in the control group, receive the novel agent; and (5), to ensure accuracy, and to preclude unconscious biases and the placebo effect, the testing process is randomized: the identities of patients receiving the active agent and those receiving the placebo, though on record, are unknown to the participants themselves and to the trial investigators (M. MaGill; "Randomized Trials"; A. Bhatt).
Neither control (arsenic or potash) nor placebo were utilized in the Middlesex Hospital trial. Nor were patients grouped according to type or stage of cancer. The paste, however, was restricted to "that class of Cancer in which there existed some form of external Tumour or Ulcer" ("Report of the Surgical Staff," 12). In addition, gender was a categorical determinant: "The chief situations of the disease, in the chosen cases, were the Female breast, and the Skin" ("Report," 12). The brevity of the trial and the etiology of cancer, however, handicapped Fell's ambitious plan. Positive results were incorrectly judged as such within too-narrow a timeframe (6 months). Whether or not the treatment had a long-term or permanent benefit could only have been discovered over time ("Report," 11).
Related Material
Bibliography
Carpenter, K. J. "The Discovery of Vitamin C." Annals of Nutrition & Metabolism. (2012) 61.3: 259-64. National Library of Science. Web. 4 February 2017.
"Cicuta." The Compact Edition of The Oxford English Dictionary, Vol. I. 2 vols. Oxford: At the Clarendon Press, 1971. 414.
Croaker, Andrew, Graham J. King, John H. Pyne, et al. Sanguinaria canadensis: Traditional Medicine, Phytochemical Composition, Biological Activities and Current Uses." International Journal of Molecular Science (27 August 2016), 17.9 ePublications SCU. Web. 23 October 2016.
Farre, Frederic John, Robert Bentley, and Robert Warrington. Manual of Materia Medica and Therapeutics: Being an Abridgement of the Late Dr. Pereira’s Elements of Materia Medica. Ed. and Pref. Horatio C. Wood, Jr. Philadelphia: Henry C. Lea, 1866. Google Books. Web. 30 December 2016.
Farrow, Ruth T. "Odyssey of an American Cancer Specialist of a Hundred Years Ago." Bulletin of the History of Medicine. (1949) 23.2: 236-252.
Fell, J. Weldon. A Treatise on Cancer, And Its Treatment. Pref. Alexander Shaw, Campbell de Morgan, Charles H. Moore, and Mitchell Henry. London: John Churchill, 1857. Google Books. Web. 22 February 2016.
"Fell, Jesse Weldon." General Alumni Catalogue of New York University, 1833-1907. New York: General Alumni Society, 1908. Internet Archive. Web. 3 February 2017.
Fetrow, Charles W., and Juan R. Avila. The Complete Guide to Herbal Medicines. Foreword, Simeon Margolies. New York and London: Simon & Schuster, 2000. 73-74.
Gupta, M., V. K. Mahajan, K. S. Mehta, and P. S. Chauhan. "Zinc Therapy in Dermatology: A Review." Dermatology Research and Practice. (10 July 2014) Hindawi Publishing. Web. 30 January 2017.
Halver, John E., and Nevin S. Scrimshaw. "Charles Glen King: 1896-1988." Biographical Memoirs (2006). Vol. 88. National Academies Press. Web. 4 February 2017.
Justamond, John Obadiah. "On the Treatment of Scirrhous Tumours or Occult Cancers." Surgical Tracts. Notes and Observations. Edited by William Houlston. London: T. Cadell, 1789. 369-383. Google Books. Web. 27 May 2016.
Lind, James. A Treatise on the Scurvy: in three parts, containing an inquiry into the nature, causes, and cure, of that disease. London: A. Millar, 1753. Internet Archive. Web. 30 January 2017.
MaGill, Marcus. “What is a randomized controlled trial in medical research?" (29 January 2016). Medical News Today. Web. 26 December 2016.
Pereira, Jonathan. The Elements of Materia Medica and Therapeutics, 1854-1857, Volume 1. 4th edition. London: Longman, Brown, Green, and Longmans, 1854. Google Books. Web. 30 December 2016.
"Randomised Trials." Cancer Research UK. Web. 30 March 2016.
Report of the Surgical Staff of the Middlesex Hospital to the Weekly Board and Governors, Upon the Treatment of Cancerous Diseases in the Hospital, On the Plan Introduced by Dr. Fell. London: John Churchill, 1857. Google Books. Web. 15 February 2016.
“Taraxacum." The Compact Edition of the Oxford English Dictionary, Vol. II. 3237.
Wood, George B., and Franklin Bache. "Sanguinaria [canadensis]; U.S.: 'Bloodroot'; puccoon." The Dispensatory of the United States of America, Part I. 9th edition. Philadelphia: Lippincott, Grambo, and Company, 1851), 646-648. Google Books. Web. January 2016.
Last modified 6 May 2021